How's Your Bedside Manner?

Tips for Improving the
Doctor-Patient Relationship
The relationship between doctors and their patients can profoundly impact medical outcomes positively or negatively.
Here are three key factors that can influence this relationship.
#1. Open Communication
Research studies prove that a physician’s ability to communicate information is every bit as important as the information itself. No wonder 65% of medical schools teach communications skills, and this training is regarded as a core competency in accreditation settings.
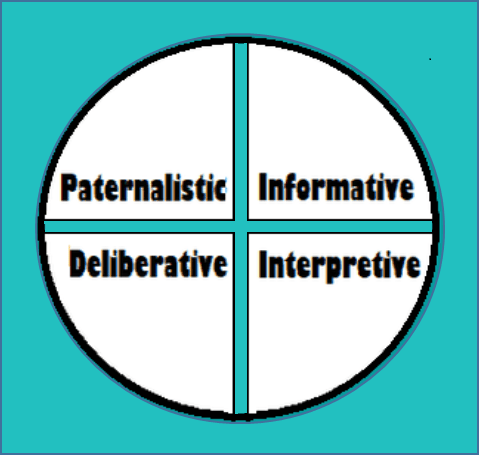
The Four Models
In 1992, two physicians, Ezekiel and Linda Emanuel, proposed four models for the doctor-patient relationship:
1. Paternalistic – The doctor acts as the patient’s guardian, promoting the patient’s wellbeing, independent of the patient’s current preferences.
2. Informative – The doctor acts as a competent technical expert, supplying relevant factual information, and implementing the patient’s chosen medical intervention.
3. Interpretive – The doctor acts as a counselor or advisor, interpreting and elucidating relevant patient values, advising the patient and implementing the patient’s selected intervention.
4. Deliberative – The doctor acts as a friend or teacher, helping the patient to determine and choose the best health-relative values that can be realized in the clinical situation.
Effective verbal and nonverbal communication can positively impact a patient’s symptoms, pain control, emotional health, and blood pressure levels. Likewise, miscommunication and a poor bedside manner can have severe negative implications.
Medical practitioners can facilitate open communication with their patients by remembering these guidelines:
- Take the time to sit down and establish eye contact with your patient.
- Listen without interrupting, so you can determine what your patient already knows.
- During examinations, explain what you’re doing and reassure your patient.
- Speak slowly and deliberately.
- Keep your explanations clear and straightforward.
- Empathize with your patient by acknowledging and validating his feelings.
- Allow your patient time to formulate his thoughts.
- Note your patient’s facial expressions and body language.
2. Shared Decision-Making
Doctors and their patients must collaborate on their medical decisions. The decision-making process should be shared with patients right from the onset. That way, all decisions will reflect the patient’s beliefs and values, not just the doctor’s medical expertise.
Even relatively small decisions should involve shared decision-making. For instance, "I can prescribe a medication to help with your symptoms, but I suspect they may go away on their own if you wait a while. Which would you prefer?"
Collaborative decision-making results in increased patient satisfaction and loyalty. Patients feel empowered in this process, enabling their doctors to provide more personalized care.
3. Doctor-Patient Trust
Trust is fundamental to any physician-patient relationship. To achieve the best medical outcome, patients must believe their doctors are working in their best interests.
A 2017 study found that a patient’s trust in his practitioner is even more critical than his satisfaction with a given medical treatment. Patients who trust their doctors feel better overall, have fewer medical complaints, and enjoy a higher quality of life.
You may be surprised that almost half of all patients fail to follow a doctor's recommended treatment. Why? Because they’re filtering these instructions through the competing demands on their time and energy, as well as their existing belief systems.
They then decide if the recommended treatment is desirable (or possible), given the demands of their everyday lives.
The patients who are more likely to follow the doctor’s recommendations and instructions are the ones who trust their physicians. These patients are also more satisfied with overall quality of care and more likely to continue with that particular care provider.
Doctor-patient trust hinges on several factors. Here are three of the most important:
- The physician’s willingness to listen,
- The patient's belief that the doctor appreciates his ability to make informed decisions, and
- The patient’s comfort level when engaging in health-related dialogue.
--Article Continues Below--
Besides actively listening and maintaining eye contact, doctors can also build trust through light touch, when appropriate. (To avoid any misinterpretation, it's usually best to do this when someone else is in the room.) A hand on the shoulder demonstrates an understanding of the patient's stress or pain.
Impact on the Future of Healthcare
Healthcare continues to become more personalized and patient-centered. In the future, the doctor-patient relationship will increasingly shape medical outcomes. Doctors can break down potential barriers to this more customized approach by understanding the factors influencing the relationship with their patients.
A physician’s bedside manner can make or break a treatment plan. How’s yours?
Sources:
Featured Image: Adobe, License Granted
Duke Personalized Health
Journal of the American Osteopathic Association
University of Washington Medicine
American Association for Physician Leadership
Recent Posts








Share On: