Are You Ready for Value-Based Healthcare?

Is VBC a Good Fit for Your
Medical Practice?
If you’re a healthcare provider, the type of care and reimbursement model you choose for your medical practice matters.
Most providers use a fee-for-service (FFS) system, where they’re paid according to the number of services they provide. With FFS, physicians are incentivized to see as many patients as possible, as quickly as possible. The more tests and procedures they prescribe, the more they are paid.
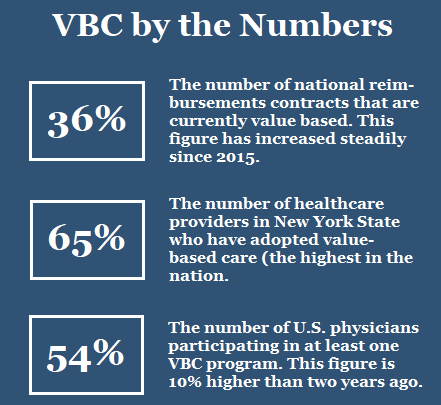
Value-based care (VBC), on the other hand, focuses on quality over quantity. VBC is rapidly becoming the wave of the future.
What Is Value-Based Care?
Value-based care is a method of motivating healthcare providers based on the quality of care as determined by their patients’ health outcomes. It’s designed to ensure that practitioners tend to their patients’ medical needs to the best of their ability -- and in as few visits as possible. The purpose of VBC is four-fold:
- Improve the quality of healthcare
- Improve the patient experience
- Reduce healthcare costs
- Improve the care team’s experience
Unlike traditional FFS, VBC is data-driven. Healthcare providers must track and report specific metrics (such as facility readmissions and population health) in order to ascertain health outcomes. Current government regulations strongly favor VBC over traditional care and reimbursement models.
VBC Payment Models
There are four main types of VBC payment models available for healthcare providers.
Accountable Care Organization
An Accountable Care Organization (ACO) is a network of care providers with varying specialties who voluntarily collaborate to offer a system of coordinated care to their patients. ACOs were originally intended for Medicare beneficiaries, but many have now expanded to include all insured patients. ACOs are designed to prevent redundant and unnecessary services, and also reduce medical errors.
When an ACO is able to provide quality care at reduced cost for patients, the savings is shared by all of the providers within the network. Of course, the opposite is also true: They all share in the losses if the quality of care is inadequate. In that regard, providers assume some financial risk when joining an ACO. Those who do not meet the VBC standard may have to repay Medicare or a private insurer.
Bundled Payments
With bundled payments, patients pay a single price for an entire episode of care, even if multiple providers are involved in the treatment. Providers are reimbursed collectively for the pre-determined costs to treat a specific condition, regardless of the number of practitioners, procedures or care settings. Payment is based on the treatment outcome.
VBC in Iowa
The state of Iowa is in the process of implementing three separate strategies to support the transition to value-based care:
- A real-time system to alert ACOs when one of their assigned members has been admitted/discharged as an inpatient, or has visited an emergency room.
- A statewide technical assistance program to help stakeholders transition to value-based payment; and
- Development of community care teams to identify and coordinate community resources that address the social determinants of health.
Source:
Change Healthcare
For example, if a patient undergoes surgery, a single payment to the surgeon, anesthesiologist and care facility would be bundled together instead of paying each provider separately. This payment would be based on historical prices.
As with ACOs, there are certain financial risks associated with bundled payments. If the treatment costs are above the target price for a particular episode of care – for example, because of medical complications -- the excess cost must be covered by the healthcare provider. Likewise, whenever treatment costs are kept below the bundled price, care providers share the savings.
Patient-Centered Medical Home
While it may sound like a place, a Patient-Centered Medical Home (PCMH) is actually a model for primary care. These groups are similar to ACOs in that they involve a collective of healthcare providers working to deliver all-inclusive medical services to their patients.
According to the U.S. Department of Health and Human Services, a PCMH is defined by five primary features:
- Comprehensiveness
- Patient-Centeredness
- Care Coordination
- Accessibility
- Quality/Safety
However, unlike an ACO, a PCMH is a care delivery model, not a reimbursement model. The PCMH offers a centralized care setting for managing all the patient’s various needs. These patients develop one-on-one relationships with their care providers. The care providers, in turn, take into account both medical and environmental considerations when identifying the patients’ needs.
The PCMH model has proven to be particularly effective in coordinating care for patients with complex chronic disease. Medical facilities can become PCMH certified through several differing accreditation programs.
--Article Continues Below--

Capitation
Capitation is another value-based payment model. With capitation, healthcare providers receive fixed fee per patient, which is paid in advance. This fee is based on various factors, such as demographic data, number of patients involved, and range of services provided. In capitation, physicians are paid whether or not the patient seeks care.
Rural communities, which often have difficulty attracting and retaining primary care providers, can particularly benefit from capitation programs. Capitation offers these providers both the flexibility to customize care for their communities and a sense of financial security.
Benefits of Value-Based Care
Should you consider adopting a value-based care for your practice? Here are some of the benefits:

VBC Challenges
One of the main challenges practitioners face when transitioning to value-based care is effectively tracking the required metrics. If they are to accurately calculate healthcare costs, providers must track a bevy of data (staffing, population health figures, clinical information, patient acuity, etc.).
Most of the technology and internal processes currently in use are designed to accommodate the fee-for-service model. So choosing the best technology partner when transitioning to VBC will be important. For a comparison of VBC services and vendors, click here.
Another common challenge concerns the organization’s internal culture, which could be resistant to adopting VBC. Providers must undergo a paradigm shift from “volume and claims” to “value and health outcomes.” Such a shift requires training and a reasonable adjustment period for a smooth transition.
Improved Patient Satisfaction
Value-based care is all about patient satisfaction. When providers offer more personalized treatment solutions, they ensure a more positive patient experience. Satisfied patients are more likely to return and/or recommend a medical practice to others.
Improved Care Coordination
In VBC, incentives and advanced technologies help coordinate care with multiple providers. Better patient outcomes result when practitioners collaborate to improve overall health.
A Healthier Society
When healthcare costs are affordable and medical providers personalize their services, patients with chronic conditions are more likely to address their medical issues early on. VBC works to create a more financially stable population that seeks treatment for chronic illnesses through the best available care methods.
The Future of Healthcare
The Department of Health and Human Services continues to offer incentives to care providers who transition to value-based payment models. (One such incentive increases the Medicare Part B base payment rate by as much as nine percent, with the possibility of additional lump sum payments.)
In the current landscape of ever-increasing healthcare costs, VBC is quickly becoming a critical part of the prudent provider’s strategy to contain costs while generating revenue.
The providers who have already started to shift their focus from care and treatment to prevention and health maintenance are positioning themselves for the future.
Sources:
Featured Image: Adobe, License Granted
RevCycle Intelligence
Health IT Analytics
Software Advice
CapMinds
Agency for Healthcare Research and Quality
Recent Posts










Share On: