The Fat of the Land: Iowa Obesity a Growing Concern

Primary Care Doctors Are Key to
Effective Treatment
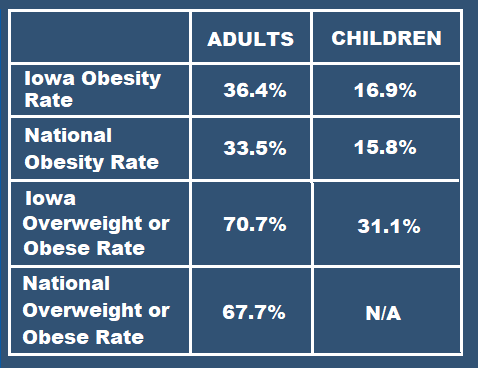
More than one-third of Iowa’s adult population is obese – 36.4 percent, to be exact, according to the latest CDC* figures. We’re now the 11th most obese state in the country.
An additional 34.3 percent of Iowans are overweight but not obese. In other words, only 29.1 percent of our state’s adult residents are within a normal weight range.
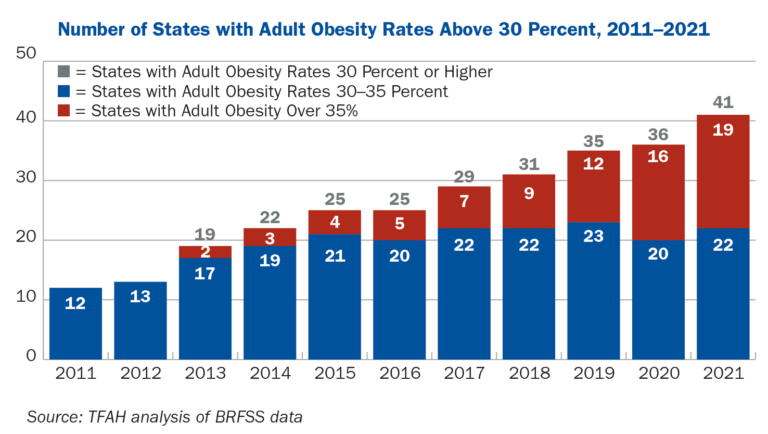
Nationwide, obesity climbed sharply during the last decade, but the highest increases occurred in only a handful of states -- including Iowa, where the rate jumped
more than eight percentage points.
* The CDC collects obesity data from two different sources. State obesity figures (reported here) are based on self-reported data from the Behavioral Risk Factor Surveillance System (BRFSS). National obesity figures use National Health and Nutrition Examination Survey (NHANES) data based on measurements taken during physical examinations. As a result, the national figures are higher and considered more accurate.
Why Here?
Obesity is a complex disease, encompassing biological, psychological and environmental factors. Even so, research indicates that too many calories and too little physical activity are most often the primary culprits. Americans as a whole consumed 20 percent more calories in 2020 than they did in 1983.
Here are some of the other factors that likely contribute to Iowa’s particularly high rating:
Rural Population
Our state’s population is still about 36 percent rural – more than double the national average. Rural areas experience higher obesity rates than the nation as a whole. These less populated communities often lack facilities and infrastructure to encourage physical activity, as well as access to affordable, healthful food. (See "Food Insecurity" below.)
And healthcare facilities located in rural areas are less likely to employ nutritionists and other weight management experts.
Food Insecurity
Almost half of the Iowans who experience food insecurity are obese. While that may appear contradictory on the surface, these residents are typically "overfed but undernourished," according to Dr. Nicole Gilg Gachiani, former chief physician at Broadlawns Medical Center in Des Moines.
Obesity Figures
at a Glance
Here's how the latest Iowa obesity statistics compare with extrapolated national data:
Many of them rely on food banks and pantries where much of the donated food is high in carbohydrates and fats but low in protein and other vital nutrients.
Prevalence of Fast Food
Iowa is among the top 10 states in the country with the
most fast-food restaurants
per capita (4.7 per 10,000 residents). Busy executives, college students, and hectic families often rely on fast food because of its convenience. Journalist and food researcher Michael Pollen estimates that 20 percent of American meals are eaten in cars.
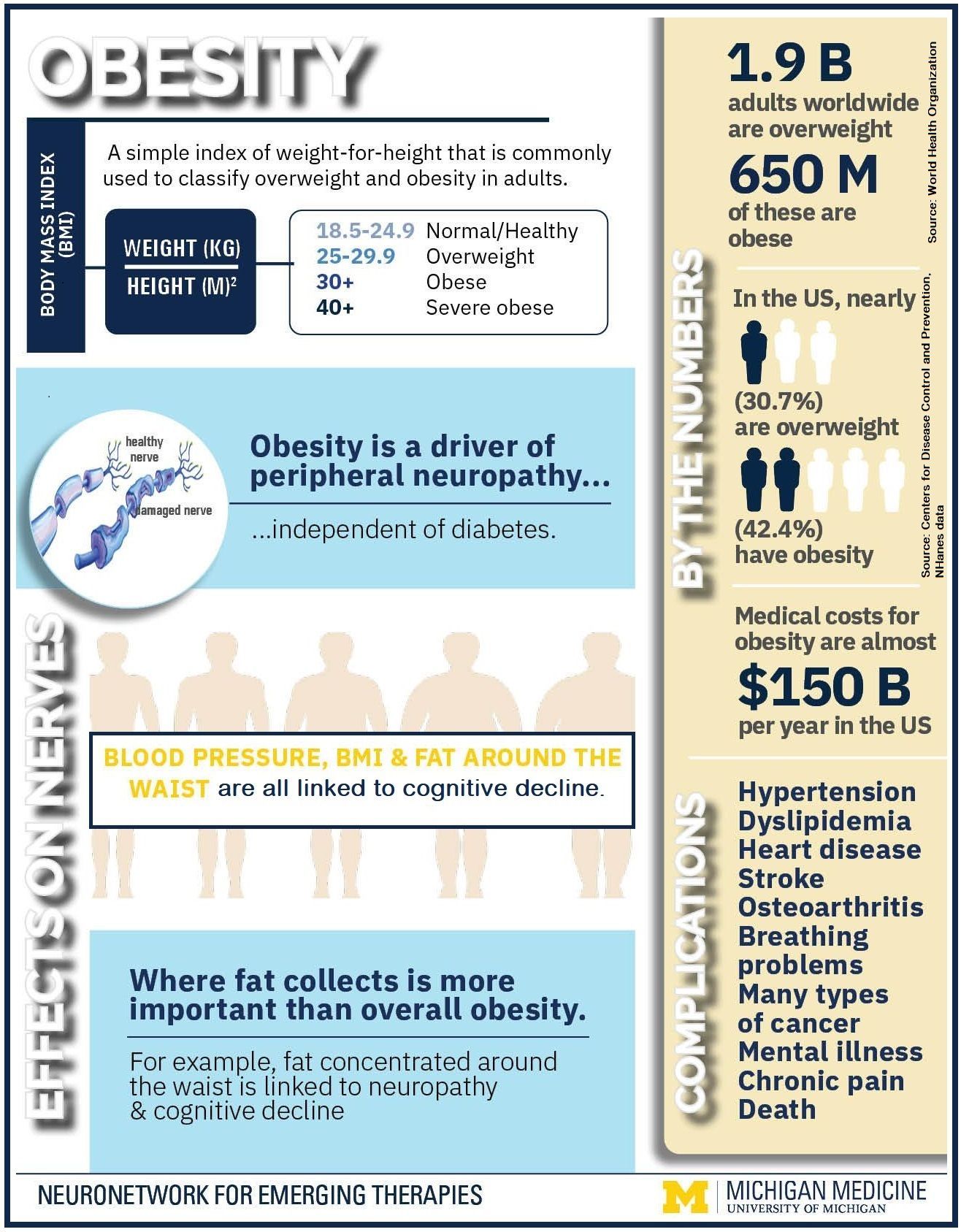
But this convenience comes with a price tag. The World Health Organization has identified a definite correlation between increased fast-food sales and higher body mass index (BMI) within a community.
Social Contagion
Then there's the social contagion factor. Research confirms that counties with a high obesity rate tend to perpetuate obesity via “social contagion.”
A 2018 USC study illustrated this phenomenon. By examining military families (who relocate frequently).
The researchers found that families assigned to installations in counties with higher obesity rates were about 25 percent more likely to become obese or overweight than those assigned to areas with lower obesity. They concluded that unhealthful eating, sedentary lifestyles, and being overweight are more socially acceptable in communities where obesity is common.
All the above factors combine to create an ideal environment for obesity to flourish. According to Rhea Farberman, policy research director at Trust for America’s Health, Iowa's obesity rate is at "crisis level."
What's Being Done?
Iowa officials have developed several programs over the years in an effort to curb the state’s obesity issue. Here are two of the most current initiatives:
--Article Continues Below--
Iowa Stops Hunger
Public and private organizations joined forces last fall and created the Iowa Stops Hunger Coalition to address food insecurity across the state. Insurers and healthcare providers are coordinating with nutrition partners to provide healthful food, nutrition education, and support in eight counties that Iowa HHS has identified as lacking reliable access to affordable, nutritious food.
Iowa Medicaid administers the coalition’s pilot program, which specifically targets mothers with young children residing in food-insecure areas.

Physician, Heal Thyself
Doctors are not immune from the obesity epidemic. A Johns Hopkins survey found that 51 percent of primary care physicians are obese or overweight.
Additional studies have shown that obese patients are less likely to accept nutrition advice from an overweight physician, and overweight physicians are less likely to offer it.
The Association of American Family Physicians (AAFP) recommends the following for overweight primary care doctors:
- Regularly visit your own physician and adopt a healthier lifestyle.
- Share your personal weight goals and achievements with your obese patients.
- Create an office environment that promotes healthy lifestyles (e.g., include healthful food options in vending machines and initiate lunchtime walking programs).
5-2-1-0 Healthy Choices Count!
Fifteen Iowa counties recently received $265,000 in government grants through the state’s 5-2-1-0 Healthy Choices Count! program, an obesity prevention initiative launched in 2017 aimed at encouraging healthful habits in school-age children. (The numbers in the program’s name refer to five servings of vegetables per day, a maximum two hours of recreational screen time, one hour of physical activity, and zero sugary drinks.)
Information about how individual communities are utilizing these grants can be found HERE.
How Doctors Can Help
The Harvard T.H. Chan School of Public Health recommends the following best practices for primary care physicians:
- Routinely measure BMI in all adult patients.
- Order appropriate lab tests for patients who are overweight or obese.
- Prescribe a long-term treatment strategy, including:
- Diet and lifestyle counseling
- Weight loss medication, when appropriate
- Bariatric surgery for severely obese individuals, when appropriate.
Healthcare providers in rural areas can also help develop obesity prevention programs within their communities.
The Rural Obesity Prevention Toolkit provides resources to help identify regional factors that promote obesity, convene partners to address those issues, and apply proven obesity prevention strategies.
Speaking With Patients About Obesity
Primary care physicians are not always comfortable addressing their patient's obesity. Weight is a very sensitive subject for many patients, but particularly the obese. However, it's an area that cannot be ignored when caring for an individual's overall health.
The following video clip offers practical advice on how to discuss obesity with patients:
Recent Posts
VISIT US
HOURS
HOURS
This communication is from a debt collection agency and is an attempt to collect a debt. Any information obtained will be used for that purpose.








Share On: